2019-20 Summary:
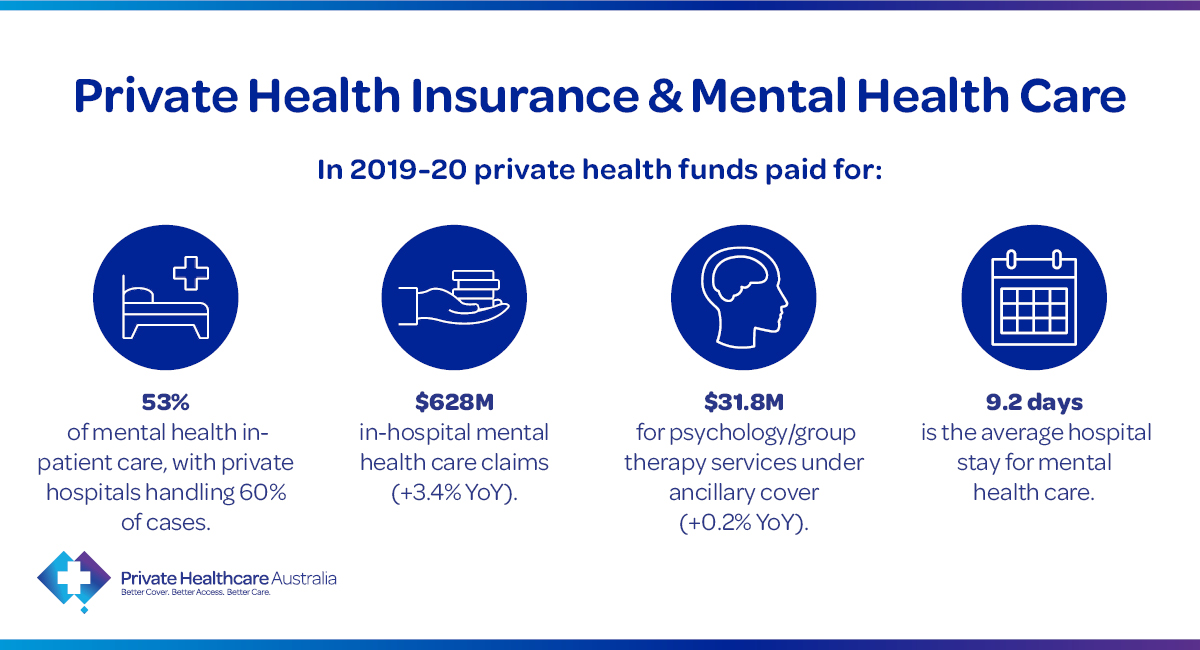
- Private Health Insurance (PHI) paid for 53% (191,428 out of 359,990) of all mental health care separations in Australian hospitals (with the private hospitals sector handling 60% of cases). (AIHW)
- Benefits paid by PHI for in-hospital mental health care claims totalled $628M (a 3.4% increase on the previous year). (DoH)
- Under extras or ancillary cover (services for out-of-hospital medical care), PHI paid an additional $31.8M in total for member’s claims for psychology/group therapy services (a 0.2% increase on the previous year). (APRA)
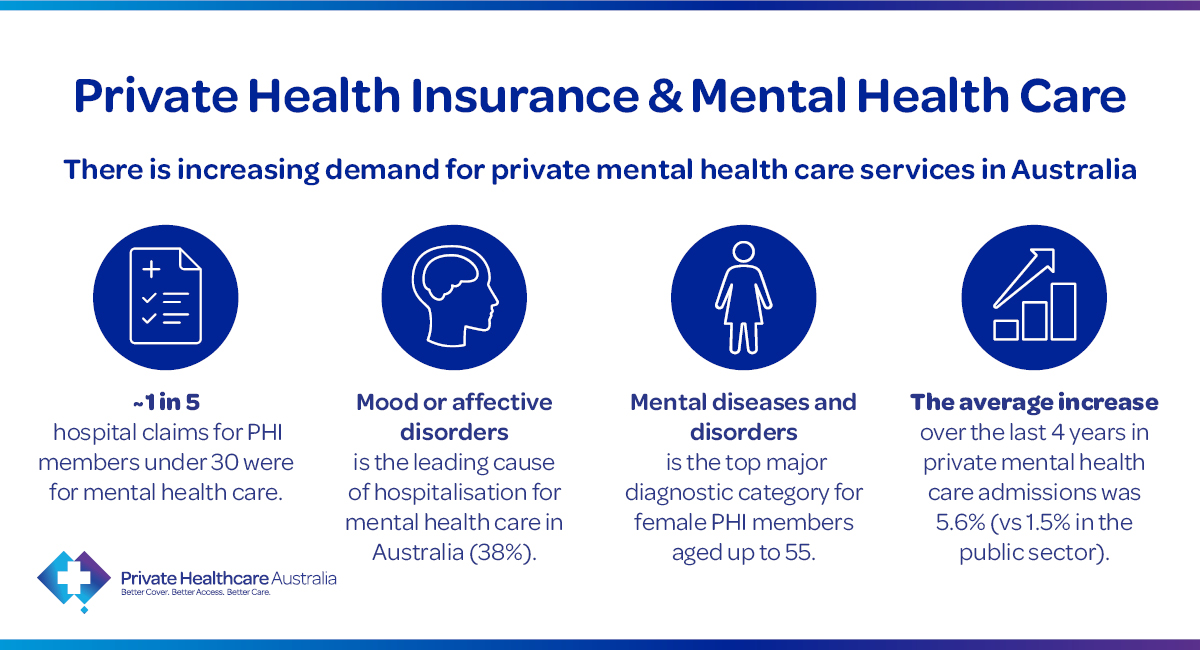
- About 1 in 5 hospital claims for PHI members under 30 were for the hospital treatment and care of patients with psychiatric, mental, addiction or behavioural disorders. (PHA)
- Mental diseases and disorders is currently the top major diagnostic category for PHI female members aged up to 55 years of age (was only previously ranked #3 as recent as 2017/18). (PHA)
- Mood or affective disorders (38%) is the leading cause of hospitalisation for mental health care treatments in Australia, followed by Neurotic, stress-related and somatoform disorders (19%). (AIHW)
- The average increase over the last 4 years (2015-16 to 2019-20) in admitted mental health care separations in the private hospitals sector has been 5.6% (compared to 1.5% in the public hospitals sector). (AIHW)
- Amongst females, the highest age group with the most mental health care hospital separations was the 20-24 group (10.7%) followed by 45-49 (9.9%) and 30-34 (9.8%). (AIHW)
- Amongst males, the highest age group with the most mental health care hospital separations was the 45-59 age group (11.4%) followed by 35-39 (11.2%) and 40-44 (11.1%). (AIHW)
- Overall, the highest age group with the most mental health care hospital separations was the 45-49 age group (10.5%) followed by 35-39 (10.2%) and 30-34 (9.9%). (AIHW)
- Females accounted for 58% of all mental health care hospital admissions; 65% for under 25s and 63% for under 30s. (AIHW)
- Overall, the average length of stay in hospital for mental health care separation is 9.2 days. (AIHW)
‘Mental Health Share’ of Australian Government private health insurance subsidies spent on hospital care
The ‘mental health share’ of Australian Government private health insurance subsidies spent on hospital care in 2018-19 was estimated by AIHW to be $159.3 million.
Total Costs of In-Hospital Mental Health Treatments over a PHI member’s lifetime
Mental health can be a multifaceted and complex disorder and treatment in hospitals can be prolonged. Under PHI, the total cumulative fund benefits paid for mental health treatments in hospitals over a PHI member’s lifetime can be as much as over $1 million (over the course of the member’s recurring visits to hospitals), whereby the member has repeated visits to hospitals for over 10 years for different mental health conditions like schizoaffective disorder, schizophrenia, recurrent depressive disorder, severe depressive episode, PTSD, bipolar disorder, eating disorder and dysthymia (a chronic form of depression). These are often conditions requiring prolonged treatment and observation in hospitals over the course of a member’s lifetime. (PHA)
Supporting mental health – waiting period exemption for higher benefits
From 1 April 2018, PHI members on a hospital policy which provides restricted benefits for psychiatric care can upgrade their cover without having to serve a two-month waiting period to access higher benefits for psychiatric care in a private hospital. This exemption applies only once per lifetime and can only be accessed if members have already completed an initial two months of membership on any level of hospital cover.
Since 1 April 2018 to 31 December 2020, over 13,500 people upgraded their insurance cover to access higher benefits for in-hospital psychiatric care treatment without serving a waiting period and claimed more than $163.9 million in benefits. (DoH)